Top Electronic Medical Record & Medical Billing services Enable Healthcare
This code-specific structure allows Medicare to adjust payment policy in response to clinical advancements, utilization trends, and cost data. CMS expanded the exclusion list to include specific remote therapeutic monitoring device supply codes related to respiratory and musculoskeletal systems. These services involve technology-enabled data collection over defined timeframes and reflect modern care delivery models beyond traditional facility-based monitoring.
National Coding Director
Small mistakes or outdated software can lead to data breaches, HIPAA violations, and fines. Staff may also be busy with many tasks, making it harder to stay up to date with rules. Controlled-access reporting systems keep financial information private while helping practices track https://takapoo.net/what-are-adjusting-entries-definition-types-and/ revenue. Chronic care management services require documented care coordination and may use specific CPT codes like or for billing monthly management.
Verify the patient’s insurance.
We code MAC cases precisely, including qualifying circumstances and ASA modifiers. This blog covers SNF Consolidated Billing exclusions for 2026 and essential Medicare rules. Practices that treat PA as a strategic function, rather than an afterthought, see measurable improvements in billing outcomes and staff satisfaction.
Boost Practice Revenue with Endocrinology Medical Billing
By addressing injuries immediately, we help you recover physically and strengthen the medical evidence that supports your claim. For example, if your attorney prepares for mediation, we can provide updated treatment summaries and billing totals in advance, strengthening your negotiation position. Patients Choice has established relationships with many personal injury law firms. This familiarity allows us to streamline communication, understand legal timelines, and anticipate documentation needs before they are requested.
How The Electronic Medical Billing Process Works
- Do you know that you can help health care organizations identify inefficiencies, optimize processes, reduce denials, and increase revenues?
- In-house billing means the practice manages all billing and coding activities internally using its own staff and systems.
- Our Accredited Revenue Cycle Management Course walks you through all the steps in revenue cycle management.
- These codes are essential for claims processing, tracking services, and ensuring accurate payment.
- The difficulty is to collect payment as it keeps everyone satisfied effectively.
- Sedation combined with local anesthesia for procedures like endoscopy or minor surgeries.
- This medical billing system makes use of certain software tools in order to help the patient complete the procedure.
Practices that embrace these capabilities set themselves up for more predictable revenue, fewer disruptions, and a stronger foundation for delivering patient care. This digital process allows providers to track claims in real time and respond to rejections or denials more quickly than with paper billing. Instead of mailing forms, the claim submission process uses electronic data interchange (EDI) to send ANSI-837 files electronically to the insurance company or clearinghouse.
Emphasize Accurate Documentation

At Transcure, we don’t just understand these problems but also solve them. Our team of 1100+ AAPC-certified coders and billers specializes in the nuanced billing of family medicine. We handle every detail, from accurate coding and clean claim submission to relentless denial management. Our end-to-end family practice RCM services ensure you capture all revenue and maintain a healthy cash flow. This is another crucial step in claim submission in medical billing.

Family Practice Revenue Cycle Management (RCM) with Transcure
Claims submitted after this deadline are at risk of immediate rejection. It’s vital for practices to be clear medical billing process on the deadlines set by each insurance provider to avoid denials and ensure timely payment. In addition, you’ll learn about account receivable, denial management, and medical billing reporting best practices.
How a Professional Billing Company Ensures HIPAA Compliance
- They get my bills paid in record time and help us to generate millions in revenue.
- It can also be critical to the success of your PIP or Med Pay claim.
- Billing personnel and coding specialists must understand coding guidelines, insurance requirements, and the ethical implications of incorrect billing.
- Additionally, they summarise other crucial data from the record, such as doctor names, dates of procedures, and other details.
- Even minor failures in the diagnostic or procedure code will lead to underpayment, delays or audit risks.
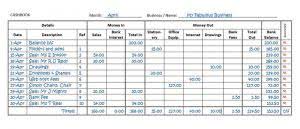
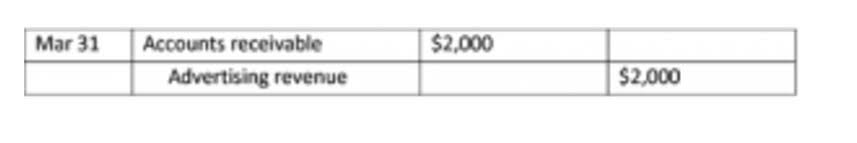
Payment processing is handled electronically, improving access to payment information and speeding up the revenue cycle. Ensure that the ICD-10 diagnosis codes and CPT procedure codes applied to the claims accurately reflect the provided services. Furthermore, you must attach operative reports, progress notes, and other records to give evidence for the medical necessity of the services billed. This is the most crucial step in Purchases Journal claim submission, as it will prevent you from submitting erroneous claims.
- In many cases, appeals are denied, resulting in lost revenue or write-offs of patient balances.
- In that case, we ensure the imaging is completed before certain therapy milestones so the therapist can adapt the treatment plan accordingly.
- This guide goes deep into how medical billing and coding actually work in real-world practice.
- Similarly, Transcure is an endocrinology medical billing company enabling practitioners to get payments on time.
Mitigating Claim Denials
Traditionally, capturing charges has been a time-consuming task for healthcare professionals, diverting their focus from patient care. Yes, our coders are trained in payer-specific billing rules, including Medicare, Medicaid, and private insurance companies. Moreover, we conduct regular training to ensure they stay updated with changing regulations. From a billing perspective, prior authorization acts as a gatekeeper. When handled correctly, it protects reimbursement and prevents avoidable denials. When mishandled, it introduces delays, rework, lost revenue, and significant administrative strain.
Recovering from an accident is physically and emotionally challenging, and dealing with insurance paperwork should not be your responsibility. Conditions such as whiplash, mild traumatic brain injury, or soft tissue damage might not cause severe symptoms immediately, but can worsen over time if left untreated. Early evaluation allows for quicker diagnosis and intervention, improving recovery outcomes and reducing long-term complications. The Texas area sees high traffic-related injuries, with busy routes often contributing to collisions. Construction zones and rush-hour congestion further increase the risk of accidents.